VisualEyes™ Support
Available Training
-
How to perform the Sinusoidal Harmonic Acceleration (SHA) test
-
How to perform the Velocity Step test
-
How to perform the Vestibulo-Ocular Reflex (VOR) Suppression test
-
How to use VisualEyes™ EyeSeeCam
-
How to perform the Dynamic Visual Acuity (DVA) test
-
How to perform the Advanced Dix-Hallpike test
-
How to perform the Supine Roll test
-
How to perform the Lempert (BBQ) Roll
-
How to perform the Gufoni Maneuver
-
How to perform the Epley Maneuver
-
How to perform the Brandt-Daroff Exercise
-
How to perform the Anterior Semont Maneuver
-
How to perform the Posterior Semont Maneuver
-
How to perform the Caloric test
-
How to perform the Optokinetic Nystagmus (OKN) test
-
How to perform the Gaze test
-
How to perform the Saccade test
-
How to perform Positional Nystagmus testing
-
How to perform the Spontaneous Nystagmus test
-
How to perform the Smooth Pursuit test
-
How to perform calibration procedures
-
How to perform the Lateral Head Roll test
-
How to perform the Subjective Visual Vertical (SVV) test
-
How to perform VORTEQ™ vHIT
-
How to perform Saccadometry
-
How to perform the Active Head Rotation test
-
How to perform the Ocular Counter Roll (OCR) test
-
How to use the Research Module
-
How to perform the Gaze Stabilization Test (GST)
-
How to perform Cervical Gaze testing
-
How to perform the Functional Vision Head Impulse Test (fvHIT™)
-
How to use keyboard shortcuts in VisualEyes™
-
How to perform Pupillometry
-
How to perform Self-Paced Saccades
-
How to perform the Smooth Pursuit Neck Torsion (SPNT) test
-
How to set up and troubleshoot monitors for oculomotor and optotype tests
How to perform the Dix-Hallpike test
What is the Dix-Hallpike test?
The Dix-Hallpike test, also referred to as the Dix-Hallpike maneuver, is a diagnostic maneuver used to identify benign paroxysmal positional vertigo (BPPV). The Dix-Hallpike test can be performed by a single clinician, who repeatedly guides the patient from a seated position to a supine position. A positive test result may be indicated by the patient reporting vertigo or if the clinician observes torsional nystagmus.
When to perform the Dix-Hallpike test?
The Dix-Hallpike test is valuable in patients with complaints of positioning vertigo. For example, in patients that get dizzy when they sit up quickly or roll over in bed.
Precautions
Before performing the Dix-Hallpike test with your patient, consider the following.
1. Past injuries
Before performing any positioning maneuver, it is important to ask if the patient has current or past injuries of the neck or spine.
2. Neurological symptoms
If neurological symptoms occur during the execution of positioning maneuvers, stop the procedure immediately and refer for a neurological evaluation. These symptoms might include:
- Confusion
- Numbness
- Blurred vision
- Weakness of the arms or legs
3. Otoconia displacement
It is important to remember that the consistency of fluid inside the vestibular system is viscous. Thus, you should allow enough time within each of the Dix-Hallpike maneuvers for the otoconia to achieve most displacement. This condition may also be responsible for a delayed onset of nystagmus.
4. Consider using VNG
It is most helpful to use videonystagmography (VNG) equipment while performing the Dix-Hallpike test. This reduces the ability of the patient to fixate during the procedure in an attempt to reduce the nystagmus. This will also allow the examiner to see even very slight torsional nystagmus.
5. Postural support
It is not unusual for the patient to lose postural control at the completion of the procedure due to the otoconia briskly falling within the cupula. It is vital that the examiner is in a stance that will provide the patient with postural support in this situation.
6. Affected ear
It is common for the patient to tell you during the intake interview which ear is affected and to describe accurately the symptoms of BPPV. Use this information to determine which ear is likely the affected ear. Always test both ears – even if the patient complains of only one side being affected.
Patient instructions
“I am going to place a mask over your goggles. I need you to cross your arms over your chest and turn your head toward me. At the count of three, I want you to lie back while keeping your head turned and your eyes open. Once you are lying down, your head will be slightly hanging down. I will help to support you through the entire process.”
Dix-Hallpike test procedure
- Begin with the patient sitting length-wise on the examination table.
- Place the Frenzel/VNG goggles on the patient.
- Have the patient turn their head to a 45-degree angle toward the side that you suspect to be affected.
- While maintaining the 45-degree head position, guide the patient in a continuous motion from sitting to lying with the head hanging off the table at approximately 20 degrees. It is imperative to provide cervical support during this part of the procedure.
- Hold this position for 30 to 60 seconds or until nystagmus has subsided.
- Guide the patient back into a sitting position.
- Allow 30 to 60 seconds in the sitting position for the patient to recover.
- Have the patient turn their head 90 degrees toward the unaffected side, so that the head is at a 45-degree angle toward the unaffected side.
- While maintaining the 45-degree head position, guide the patient in a continuous motion from sitting to lying with the head hanging off the table at approximately 20 degrees. It is imperative to provide cervical support during this part of the procedure.
- Hold this position for 30 to 60 seconds or until nystagmus has subsided.
- Guide the patient back into a sitting position.
- Maintain postural support until the patient is stable.
Example: Dix-Hallpike test performed to the right
Begin with the patient seated – wearing goggles – with their head turned 45 degrees to the right.

Quickly lie the patient back with their head turned 45 degrees and hanging approximately 20 degrees.

Example: Dix-Hallpike test performed to the left
Begin with the patient seated – wearing goggles – with their head turned 45 degrees to the left.

Quickly lie the patient back with their head turned 45 degrees and hanging approximately 20 degrees.

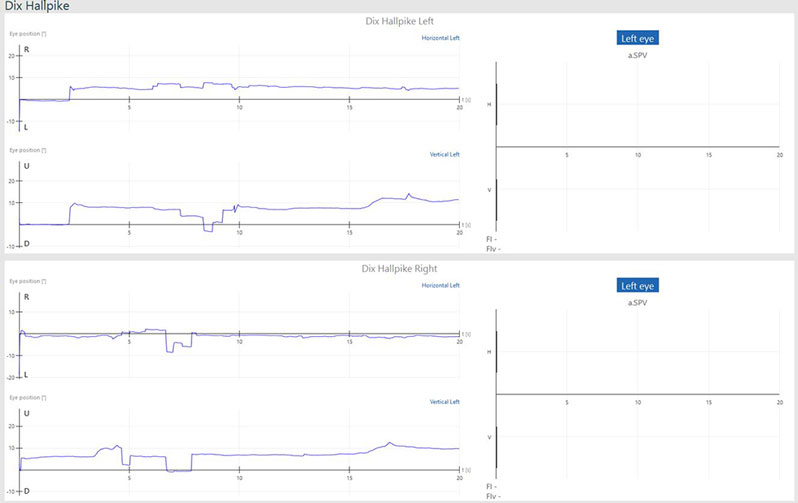
Normal Dix-Hallpike results
If the patient does not have any form of positioning vertigo, the tracing will be an almost straight line (normal eye movement is expected). The bar graphs for left and right beating nystagmus and down and up beating nystagmus will display as zero for all conditions (Figure 5).
Abnormal Dix-Hallpike results
If the patient presents with nystagmus, it is important to watch the eye video recording for several characteristics to differentiate BPPV from other vestibular pathologies.
Generally, the following characteristics will present together as a sign of BPPV:
- Does the nystagmus have a delayed onset of 2 to 20 seconds?
- Is the nystagmus a torsional (‘rotary’) nystagmus?
- Does the nystagmus fatigue after a few seconds?
- Does the nystagmus reverse direction when you return the patient to a sitting position?
- Is the nystagmus less intense upon retest?
If nystagmus is present, but does not meet these characteristics, there is a greater likelihood that a different peripheral vestibular dysfunction may be the source of the nystagmus.
If BPPV is present, nystagmus will be present in the horizontal and vertical channels. The nystagmus is represented by the triangles or green segments in the tracing and the averaged values for the strongest 10 seconds are shown in the bar graphs to the right of each tracing for each test (Figure 6).

More reading
[1] Jacobson GP, Shepard NT. Balance Functional Assessment and Management, 2nd Ed. San Diego; Plural Publishing, 2015.
[2] Dix MR, Hallpike CS. The pathology symptomatology and diagnosis of certain common disorders of the vestibular system. Proc R Soc Med. 1952 Jun;45(6):341-54. PMID: 14941845; PMCID: PMC1987487.
[3] Hughes CA, Proctor L. Benign paroxysmal positional vertigo. Laryngoscope. 1997 May;107(5):607-13. doi: 10.1097/00005537-199705000-00010. PMID: 9149161.
