Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Functional Assessment and Rehab
Dynamic Visual Acuity (DVA) Test
Description
This article introduces the dynamic visual acuity (DVA) test and its role in assessing vestibular compensation.
Table of contents
- Visual acuity
- Pathophysiology of dynamic visual acuity
- Clinical applications of dynamic visual acuity
- Bedside DVA
- Computerized DVA
- Typical DVA results
- Abnormal DVA results
- Gaze stabilization test (GST)
Visual acuity
Patients with vestibular abnormalities often complain of loss of visual acuity during head movements. This symptom is caused by vestibulo-ocular reflex (VOR) dysfunction. In these patients, the VOR is no longer able to generate fully compensatory eye movements, which results in the slippage of the image and loss of visual acuity during head movements.
Visual acuity during head movements improves with vestibular compensation. So, the aim of DVA testing is to compare visual acuity for when the head is still with the visual acuity for when the head is moving. The test can then be used to evaluate the level of vestibular compensation.
Pathophysiology of dynamic visual acuity
The vestibular system essentially behaves as a three-dimensional scale. The changes in the balance between the two sides tell us about the direction and amplitude of head movements. For simplicity, only the head movements in the plane of the lateral semicircular canals will be considered.
When the head is at rest, the tonic neural activity from the right and left sides are equal. When the head moves to one direction, neural activities from that side increase and neural activities from the opposite side decrease. The faster the head moves, the bigger the difference in neural firings from each side.
The information about head movements is sent to the vestibular and oculomotor nuclei, which is used by the VOR to move the eyes with the same velocity as the head, but in the opposite direction. As a result, the retinal slip will be minimized, which is necessary to have a clear vision during head movements.
Static compensation
Immediately after a unilateral vestibular loss, the neural firings from the damaged side decrease. The patient perceives the head moving toward the intact side and experiences vertigo and nausea. This is manifested as spontaneous nystagmus with fast phases beating away from the side of lesion. DVA testing is not particularly helpful for patients in this stage of lesion.
Over the course of several days, the tonic neural firing is restored to the damaged side and the patient's spontaneous nystagmus disappears. This results in a reduction in the patient’s symptoms as long as the head remains still. This is a milestone in the recovery of the patient, and it represents static compensation.
Dynamic compensation
In patients with a unilateral loss of vestibular function, when the head moves, neural firings change only half as much. As a result, head movements are underestimated. That means the eye velocity is also half as large as the head velocity. Because the eye movements are not fully compensatory, the eyes do not remain stationary in space during head movements.
The mismatch between head and eye velocities causes retinal slip. The images do not stay stationary on the retina and become blurry during head movements. In other words, dynamic visual acuity deteriorates because of retinal slip.
The amplitude of retinal slip can be reduced if the brain learns the new pattern of neural firing and moves the eyes faster in response to head movements. This is the next milestone in recovery, and it represents dynamic compensation. It is not known if dynamic compensation can fully restore visual acuity or just improve it.
X1 and X2 VOR rehabilitation exercises
Rehabilitation specialists use head-eye coordination exercises such as X1 and X2 exercises, which promote dynamic compensation through adaptation and central reprogramming of vestibular pathways. X1 and X2 exercises are basically gaze stabilization exercises that can improve coordination of head and eye movements.
The therapist usually sends the patient home with the description of what he or she is supposed to do. The patient is instructed to focus on a target such as a business card with writing on it and to hold this card at arm's length. The patient is supposed to start moving the head side to side slowly and then increase the velocity to the point where the writing starts to get blurry. The patient is instructed to stay at this velocity for several seconds and the exercise should be repeated a few times. The aim is that the head velocity where things become blurry increases over time and the patient's dynamic visual acuity improves.
In the X1 part of the exercise, the target (business card) is stationary and can be held or affixed to the wall. In the X2 exercises, the patient usually holds the card at arm's length and moves it either in the same direction with the head or in the opposite direction. The head movements are usually prescribed for both horizontal and vertical planes. In rare occasions, movements in the role plane are also included.
Retinal slip toward the side of lesion
For higher head velocities, the mismatch between the head and eye velocities is worse when the head moves toward the side of lesion. The reason is that when neural firings reach zero, they cannot decrease no matter how much the head velocity increases. That means dynamic visual acuity is more severely affected when the head moves toward the side of lesion.
Severe bilateral vestibular lesions
In patients who suffer from severe bilateral vestibular lesions, the VOR function is mostly impaired. In these patients, head movements cause large retinal slips and result in severe deterioration of visual acuity. Interestingly, therapists often use the same X1 and X2 head-eye coordination exercises. But instead of adaptation of vestibular pathways, the aim is to promote substitution of vestibular sensors with oculomotor and neck receptors.
Clinical applications of dynamic visual acuity
This brings us to the dynamic visual acuity (DVA) test. Traditional vestibular tests such as the caloric test, vHIT, and VEMPs are used to identify the presence of pathology. They are considered diagnostic, ‘site‑of‑lesion’ tests.
That's useful because the test results remain essentially the same as long as the pathology is stable. But they do not give any indication of the level of patient compensation. DVA is one of the few tests where the test results can change with the level of compensation and – in fact – it may be the only test that examines VOR compensation.
DVA can document impairment, and it’s very important to differentiate that from pathology. In other words, patients with the same pathology can have low or high impairment based on the level of compensation. This makes DVA a good tool to assess the effectiveness of rehabilitation and exercise-based therapies.
Bedside DVA
The early versions of DVA relied on testing that did not involve any instrumentation.
Static visual acuity
In the non‑instrumented – or bedside – DVA, the patient is seated at the prescribed distance from an eye chart. The examiner asks the patient to read the lowest line without moving the head. This provides the static visual acuity, sometimes called the baseline visual acuity. This can confuse the patient, because they expect this value to match what they get in the standard eye exam with an optometrist or ophthalmologist. It often doesn’t as the test can be performed with glasses.
Dynamic visual acuity
The next step is to ask the patient to read the lowest recognizable line during head movements. This determines the dynamic visual acuity. In normal individuals, visual acuity decreases by fewer than two lines during head movements. After an acute vestibular loss, visual acuity deteriorates significantly during head movements, sometimes by as much as six lines or more. But the performance improves over time due to dynamic compensation, which reduces retinal slip and improves dynamic visual acuity.
Active vs passive head movements
Head movements can be performed actively (by the patient) or passively (by the clinician). There's a difference of opinion if the two methods produce different results and – if so – which one is better. Passive testing seems to produce more repeatable results. But as long as one method is used consistently, the results can be compared over time and interpreted effectively.
Head rotation frequency
The prescribed head rotations in the bedside DVA are sinusoidal with a frequency of about two hertz or two cycles per second. That means the head moves from one side to the other and back to the starting point in half a second. Usually, a metronome is used to synchronize the head movements.
The problem is that the input to the vestibular system is the head velocity and not the frequency. So, the peak velocity can vary significantly depending on the amplitude of head movements. For example, if you move your head at plus/minus 10 degrees, the peak velocity is about 125 degrees per second. If you move your head at plus/minus 30 degrees, the peak velocity is closer to 375 degrees per second.
Head movement planes
In DVA testing, the head movements can be performed in the horizontal (yaw), vertical (pitch), or roll planes.
Limitations of bedside DVA
There are a couple of limitations associated with the bedside DVA test.
One of the major limitations is that the letters are visible during the entire head movement. As the head velocity varies throughout the head rotation, the patient can try to read the letters during the slow parts of the head movement.
The other limitation is that the bedside test does not differentiate between the visual acuity for movements toward or away from the side of lesion. As described above, there's a difference in the dynamic visual acuity for the two sides in patients with unilateral vestibular loss, rendering the bedside test inappropriate.
Computerized DVA
In the computerized DVA test, the patient is seated at the prescribed distance from a computer screen. The patient wears an inertial measurement unit (IMU) that can measure the head movements in three dimensions. The older IMUs were wired but the new versions are wireless, which is preferable because it doesn't restrict head movements.
Visual stimuli
In place of the eye chart, the computer displays images that the patient needs to identify. The images can be letters, words, or – most commonly – optotypes. Typical optotypes include the Tumbling E or Landolt C, where the patient is asked to identify the direction of the optotype (up, down, right, or left). The process of inputting the data can be done by the patient or by the clinician.
Static visual acuity
Before determining the dynamic visual acuity, the computerized system first determines the static visual acuity, which is the visual acuity with the head at rest. In the computerized version of the test, an optotype is displayed and reduced in size until the point where the patient can no longer identify which direction it is pointing. A threshold algorithm is used to identify the smallest optotype they can correctly identify, and this is then set as the static visual acuity.
Performing computerized DVA
For dynamic visual acuity, the computerized system keeps track of the head velocity and displays the optotype only when the velocity is within the prescribed range. As described above, the head movements can be performed actively or passively.
During the test, the patient is asked to identify the direction or orientation of the optotype. Very similar to what one goes through during an eye exam, the computer reduces or enlarges the size of the optotype if the patient correctly identifies the direction in the previous trial. A threshold search algorithm determines the limit of visual acuity based on the entire profile of correct and incorrect answers.
Typical DVA results
Figure 1 shows the DVA results for a person with normal dynamic visual acuity.
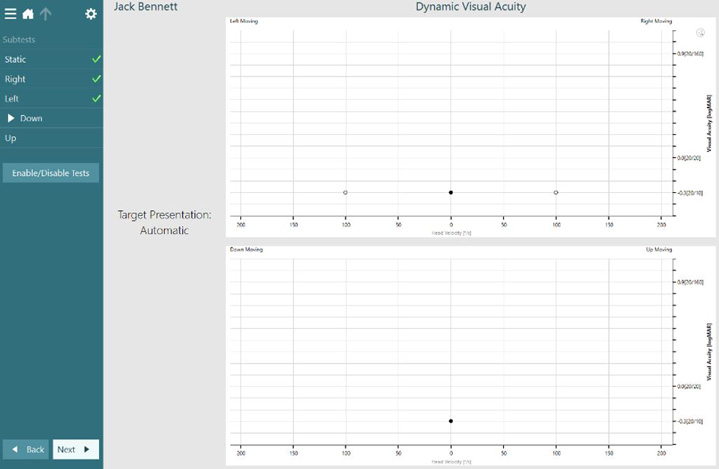
The graph displays visual acuity as a function of head velocity. The black filled circle represents the patient’s static visual acuity and the dynamic visual acuity to the right and left is represented by the clear circles. As the test was performed at a head speed of 100 degrees per second, you can see the visual acuity for the dynamic portions of the test plotted at this point along the x axis. The visual acuity is plotted on the y axis.
In this example, it remains the same for all three conditions, both static and dynamic. In individuals with a normally functioning VOR, the static acuity should not increase by more than two lines on the y axis.
Abnormal DVA results
Figure 2 shows the results from a patient who has a left vestibular lesion.

In this example, the visual acuity is reduced by greater than two lines when moving the head to the right and to the left, with the largest acuity loss with head movements to the left. This is represented by an increased LogMAR plotted on the y axis. This is indicative of a left lesion.
Figures 3, 4, and 5 show the DVA results for this patient over the course of rehab therapy.



Before rehab, the leftward DVA is significantly worse, but it improves over time with therapy. This is really the most important feature of DVA, because it tells you the level of impairment independent of the level of lesion. When you combine it with something like the vHIT, you can get both the presence of a lesion and also the level of compensation.
Related course: Objectifying the functional assessment of the dizzy patient
Gaze stabilization test (GST)
There's a companion test called the gaze stabilization test (GST), which some systems provide. GST is often performed with – or in place of – the DVA test. It determines the head velocity that causes significant deterioration of visual acuity.
GST vs DVA
The main difference is that in GST, the letter size is kept the same and the head velocity is changed, and vice versa for DVA. The head velocity can range from as low as 30 degrees per second to as high as 300 degrees per second.
The benefit of GST is that it can compare an individual's performance with the expected demands of daily activities. For example, patients whose GST results are lower than 80 to 85 degrees per second are at risk of falling. Alternatively, GST can be used for individuals who are involved in higher demand activities, such as in sports or certain occupations.
Another benefit is that the therapist can prescribe head‑eye coordination exercises most appropriate for the patient. For example, in a patient with GST results of 120 degrees per second, you want to start the head‑eye coordination exercises right around or slightly below that value and push that up as the patient progresses.
Summary
To summarize, the computerized DVA test and GST provide objective tools for assessing the VOR function in different planes. Unlike the diagnostic tests of vestibular function, the DVA test can document the impairment and the level of vestibular compensation.
The results of DVA and GST can be used to optimize the therapy protocol. For example, head-eye coordination exercises can be designed to gradually increase the GST threshold. The user can select the direction and head velocities that allow for targeted training.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
