Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Functional Assessment and Rehab
Sensory Organization Test (SOT)
Description
Table of contents
- What is the Sensory Organization Test (SOT)?
- What does the SOT assess?
- Who should you assess using the SOT?
- SOT procedure
- SOT results
- Clinical applications of the SOT
What is the Sensory Organization Test (SOT)?
The SOT is a subtest of posturography that is designed to quantitatively assess an individual’s ability to use sensory (visual, proprioceptive and vestibular) cues to maintain postural stability in stance (Clendaniel, 2000) [1].
It is not a diagnostic test to localize the origin site of dysfunction, but it complements the results of diagnostic vestibular testing by assessing the functioning of the sensory inputs into the nervous system. It is performed using a dynamic posturography force plate and visual surrounding, such as a fully immersive virtual reality (VR) headset
In the test, the patient will stand on a dynamic force plate and complete six different conditions, each with a unique combination of visual and force plate changes to challenge the balance system. The posturography force plate will measure, analyze and quantify postural sway and compare it against a set of normative data.
The test results offer an objective evaluation of a patient’s sensory processing, as well as how these systems interact within the brain and relay information to the body to maintain postural control. It can reveal if a patient has integration deficits in one or more sensory systems and can provide insights into a patient’s overall body alignment and balance strategy in normal and conflicting balance conditions. This is all essential knowledge when creating and implementing personalized rehabilitation programs.
Lastly, you can use the SOT as a follow-up tool to re-assess the patient’s functional status and progression in therapy with objective data.
What does the SOT assess?
The SOT assesses how an individual’s sensory systems are integrated for postural control. Each person has sensory inputs from three systems:
- Visual
- Vestibular
- Somatosensory
These provide information back to the nervous system to establish an internal map of body position and its relationship to the external environment. These three sensory inputs work together on multiple levels in the nervous system to provide continuous feedback and feedforward responses to produce appropriate postural control [4].
Visual system
The visual system is responsible for measuring head and eye position relative to the environment. It does this by providing information to the nervous system on details of an individual’s environment and how their body is oriented compared to those details. This system produces slower responses to maintain upright posture compared to the vestibular system [4].
Vestibular system
The vestibular system is responsible for measuring head position relative to gravity and head motion relative to self. This system produces fast responses to control eye and neck movements and longer latency responses to control movements needed to maintain upright posture. When integrated appropriately with other sensory inputs, it also provides a sense of self versus external movement [4].
Somatosensory system
The somatosensory system is responsible for measuring limb and trunk position relative to the surface by the musculoskeletal system that provides information on body position. Through multiple ascending sensory pathways, this system can assist in producing fast and sensitive responses needed to maintain upright posture [4].
SOT conditions
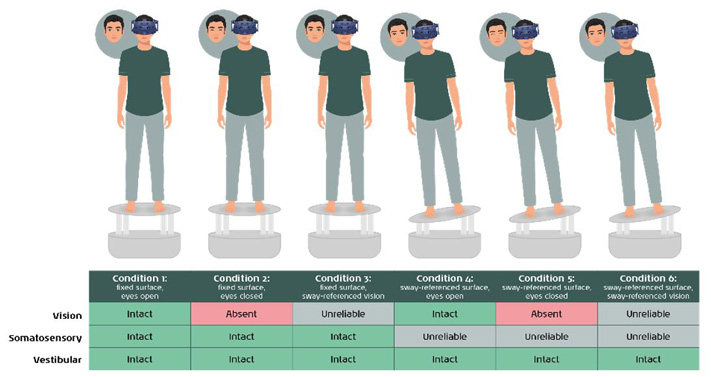
The SOT assesses how all three of these sensory systems are integrated in the central nervous system by placing an individual under six varying sensory conditions. Below is a table showing these six conditions and which sensory systems are intact, absent or producing unreliable information to the central nervous system (Figure 1).
Who should you assess using the SOT?
You can test any adult patient with balance or functional deficits, including instability or dizziness symptoms, with the SOT. You can use it to assess patients with weights up to 200 kg. If the patient is unable to stand still and unsupported, then this test is not recommended.
SOT procedure
The SOT is made up of six different conditions. For each condition, it is recommended to perform at least two trials to have an average score computed. Each trial is set at a time of 20 seconds.
Preparation for testing
Before testing, you should perform the following steps:
- Enter the patient’s age and height into the system for correct setup and comparison to normative data.
- Patients should have shoes removed (barefoot or in socks) to allow for standardized input of the somatosensory system.
- If applicable, use a safety harness on the patient. Make sure the carabiners are set at or below the level of the patient’s shoulders to prevent extra positioning input into the patient’s system.
- Center the patient's feet on the force plate. The front edge of the medial malleolus of each foot should be directly centered on the horizontal line of the force platform. The outer edge of the foot should be aligned with the antero-posterior line corresponding to the patient’s height (inner line: less than 55 inches; middle line: 56 to 65 inches; outer line: more than 65 inches) (Figure 2).
- Assist patient with donning and fitting the VR headset for comfort.
- Patient’s arms at side of body (Figure 3).


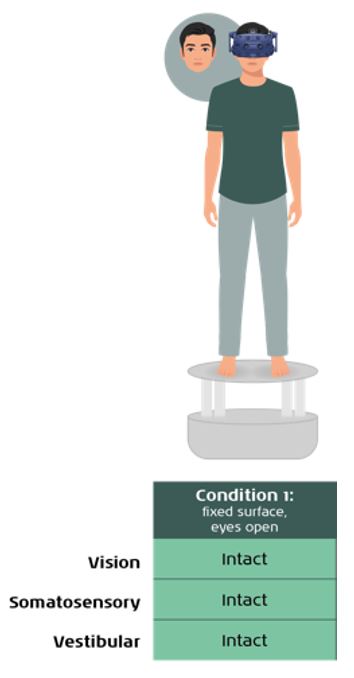
Condition 1
The test will begin with the first trial in condition one, which is a stable force plate and stable vision (Figure 4). This serves an individual’s baseline performance when all three sensory systems provide accurate input. A normal response would be very minimal sway over the 20 second trial.
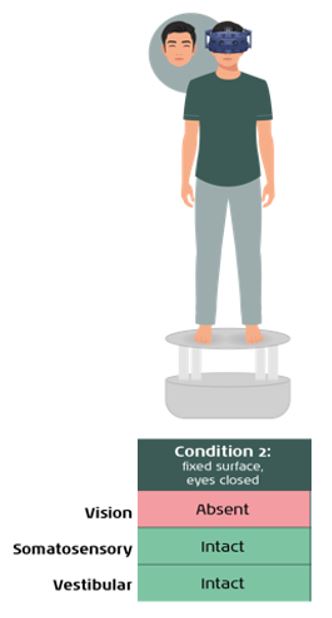
Condition 2
The test will continue to condition two, which is a stable force plate, but absent vision (Figure 5). You are now testing the individual’s postural response when the brain cannot use vision. A normal response would be slightly increased sway compared to condition one, but ability to maintain upright stance.
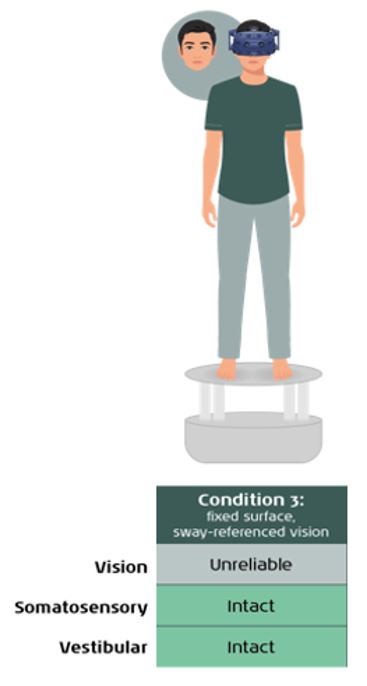
Condition 3
Next will be condition three, which is a stable force plate, but with sway-referenced vision (Figure 6). Sway-referenced vision is completed with unreliable visual cues based on the individual’s sway response.
A normal response would be the same sway compared to condition two. If a patient has increased sway, then this could indicate a visual preference, as they do not have the ability to suppress visual cues when they are unreliable.
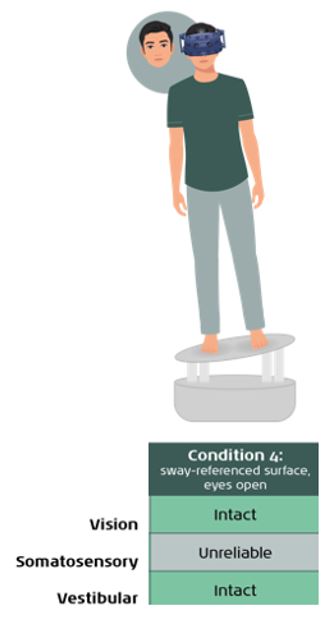
Conditions 4 to 6
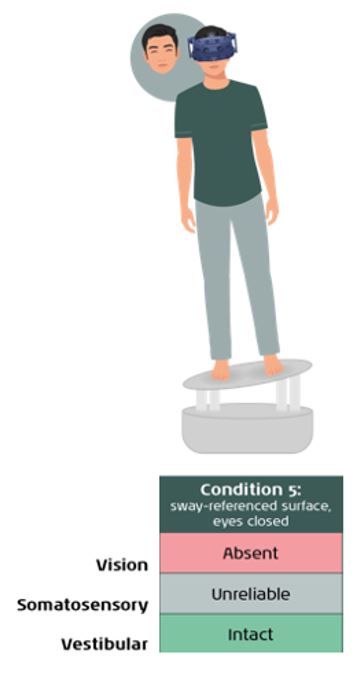
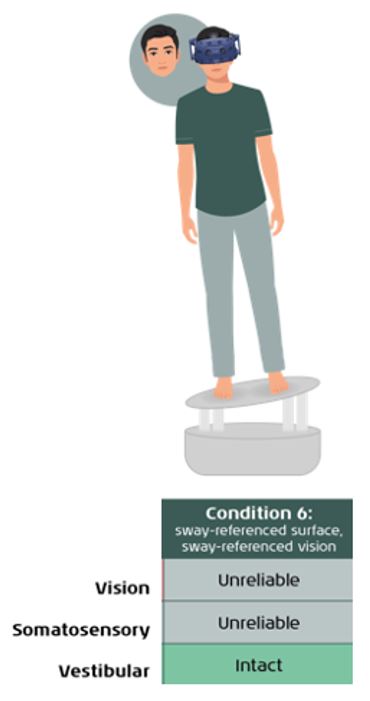
On conditions four through six, the force plate will be dynamic and provide a sway-referenced surface. This will result in an unreliable somatosensory input for the final three conditions.
Condition four includes this sway-referenced force plate with stable vision (Figure 7). A normal response would be an increased sway compared to conditions one through three, but still can maintain an upright stance.
The final two conditions both have the sway-referenced force plate, but the difference is in the visual input provided. Condition five has absent vision (Figure 8) and condition six has unreliable vision (Figure 9). For both conditions, you are now testing an individual’s balance system with the only accurate input being from the vestibular system.
A normal response for both conditions would be an increased sway compared to condition four, but still can maintain an upright stance. Similar to condition three, if a patient has an increased sway on condition six, this could indicate a visual preference.
You can watch a video of the SOT being performed below.
SOT results
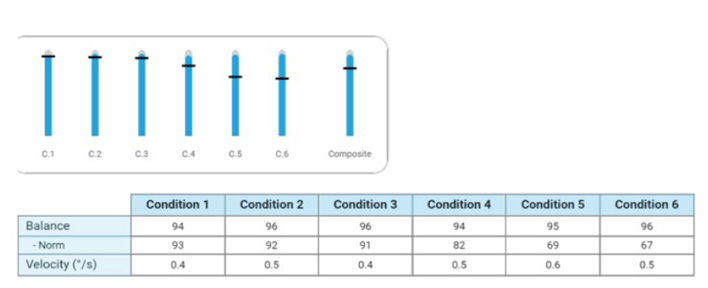
Following the SOT, the postural sway responses from all six conditions are extracted. The main report is generated with equilibrium and composite scores, sensory analysis ratios, center of pressure, and balance strategy.
Equilibrium score
This score is represented as the average sway for each of the six conditions and is compared to age-matched normative data. In the objective data table, the sway velocity (degrees per second) is also listed (Figure 10).
Composite score
This score is a weighted average of sway for all the six conditions and is compared to an age-matched score.
Sensory analysis ratios
Represented as average scores of specific conditions to identify functional impairments in the somatosensory, visual and/or vestibular systems, as well as to indicate if a patient has a visual preference (Figure 11).
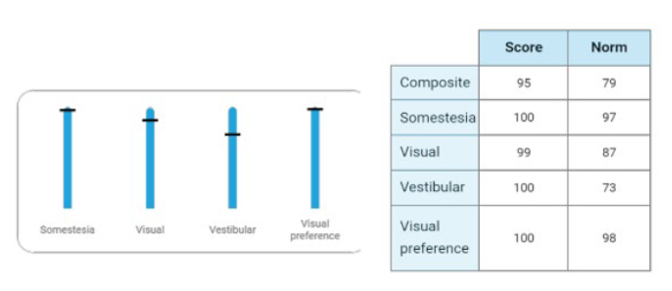
Center of pressure (CoP)
Represented as average CoP for each condition. Perfect CoP would be centered on the two lines in the graph below (Figure 12).
Balance strategy
Under dynamic conditions, the body is brought back to upright posture through certain movement strategies: ankle, hip or stepping. On the SOT, this is represented by a hip or ankle strategy based on the average equilibrium score of each condition.
The higher scores are represented as the patient using an ankle strategy since they had a higher equilibrium score and less overall sway.
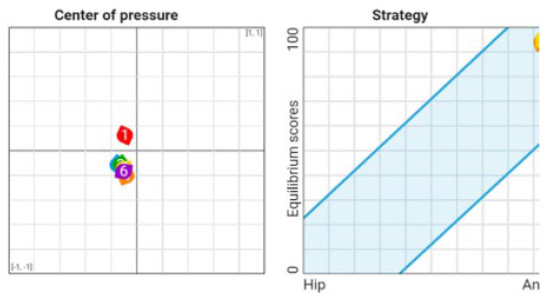
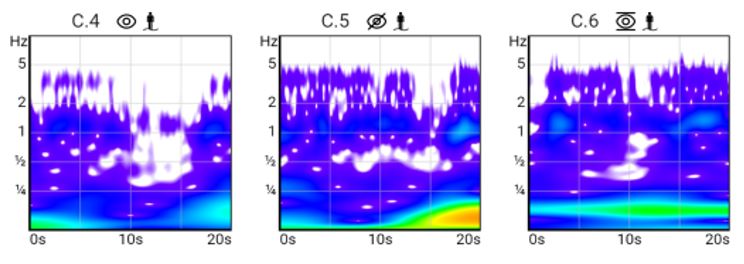
Additional graphs available include sway tracing, sway curve, wavelets and polars. These can provide further insight into how the patient performed under the six conditions of the SOT and allow for personalized rehabilitation programs.
A recent study showed the use of wavelet graphs to demonstrate the amount of energy spent to control the patient’s posture following early versus late vestibular rehabilitation in patients with unilateral vestibular loss [3].
The use of this type of graph can be beneficial to continue to guide rehabilitation programs as function compensates and objective scores normalize (Figure 13).
Clinical applications of the SOT
The SOT is one assessment of the three Computerized Dynamic Posturography (CDP) assessments:
- SOT
- Adaptation Test (ADT)
- Motor Control Test (MCT)
It is important to perform all three assessments for a comprehensive picture of your patient with a balance disorder. Remember, these assessments are not diagnostic but can help you decide if you need to refer for additional testing and how to personalize your patient’s training program.
The SOT can provide multiple points of data to guide personalized rehabilitation programs due to its ability to functionally assess the sensory inputs and provide a patient’s resultant postural response.
Sensory patterns of dysfunction
Research has supported different sensory patterns depending on which conditions are normal versus abnormal. Commonly used patterns include [2, 7]:
- Vestibular pattern (abnormal conditions 5 and 6), which can be seen in patients with uncompensated vestibular disorders, bilateral peripheral vestibular loss, or dysfunction in the vestibular pathways involving the brainstem/cerebellum.
- Visual vestibular pattern (abnormal conditions 4, 5 and 6), which can be seen in patients who have instability when somatosensory input is unreliable.
- Severe pattern (abnormal on more than conditions 4, 5 and 6), which can be seen in patients with multifactorial sensory deficits.
Using these sensory patterns of dysfunction can help a clinician structure the primary focus of their sensory integration therapeutic interventions.
Monitoring effects of vestibular rehabilitation in patients with vestibular disorders
The SOT is a valuable tool for evaluating the impact of vestibular rehabilitation, as it provides objective data to track patient progress over time. Improvements in sensory organization and a reduction in symptoms are typically expected with consistent participation in rehabilitation.
For patients with stable lesions, such as vestibular neuritis, SOT data can inform decisions about the appropriate timing for discharge from rehabilitation. In cases of fluctuating lesions, such as Meniere’s Disease, repeated SOT assessments over time can provide insights into the patient’s functional status. Research indicates temporary correlations between SOT results, Meniere’s Disease activity, and audiometric findings [8].
The SOT is also effective in evaluating function before and after surgical interventions, such as Acoustic Neuroma (AN) resections. Despite the slow tumor growth and central compensation mechanisms, patients with AN tend to score lower on SOT conditions 5 and 6 compared to healthy individuals. Post-surgery, the SOT can be used to monitor compensation and measure the effectiveness of rehabilitation. Evidence suggests that SOT scores improve over time when compared to preoperative and immediate postoperative periods [8].
Use of CDP assessments in neurological disorders
Vertigo and postural instability can arise not only from vestibular disorders but also from neurological conditions such as stroke, multiple sclerosis (MS), polyneuropathy, myelopathy, cerebellar disorders, and Parkinson’s disease. Research supports the integration of computerized dynamic posturography (CDP) with vestibular function testing as an effective diagnostic approach for distinguishing central from peripheral causes of vertigo and balance disorders [8].
Beyond aiding in diagnosis, CDP serves as a valuable tool in rehabilitation. Many patients with these conditions are at an increased risk of falling. Clinicians can leverage objective data from CDP assessments to educate patients and develop tailored fall prevention strategies.
For instance, one study highlights a strong correlation between the composite equilibrium score on the SOT and subjective scores on the Activities-Specific Balance Confidence (ABC) scale in patients with Parkinson’s disease [6].
Similarly, research indicates that CDP has greater sensitivity than the Romberg test for assessing and monitoring balance in patients with multiple sclerosis [5].
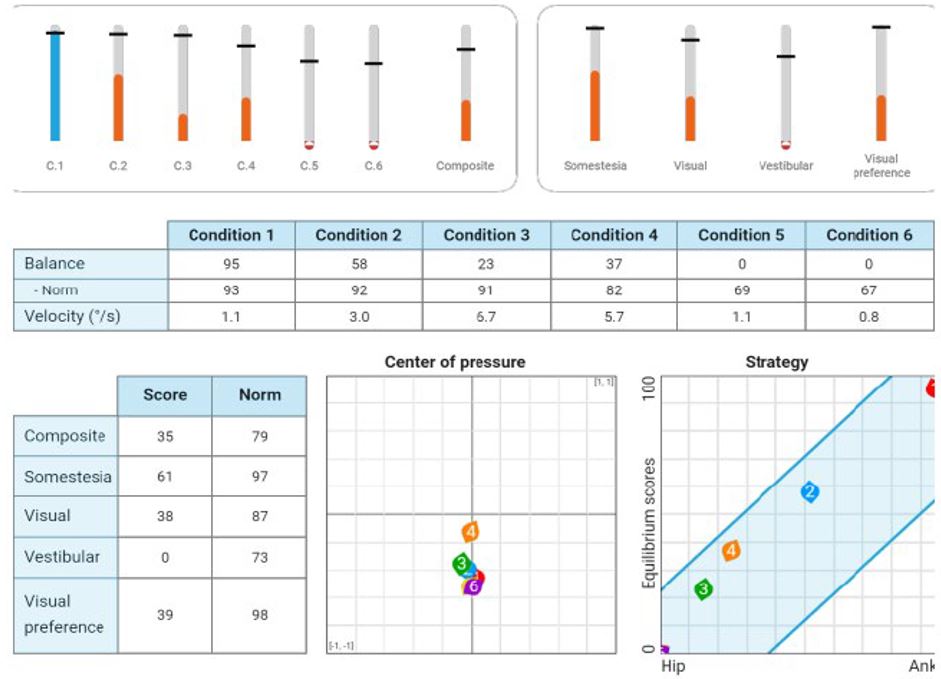
Use of SOT in functional disorders
Clinicians can use SOT results to evaluate functional disorders. In a typical SOT outcome, equilibrium scores decrease as conditions become progressively more challenging. However, patients with functional disorders may show an abnormal pattern, such as higher equilibrium scores on more difficult conditions (conditions 4 to 6) and lower scores on easier ones (conditions 1 to 3), accompanied by inconsistent sway patterns and atypical balance strategies [8].
Clinicians should exercise caution, as functional disorders often coexist with other conditions. For example, patients with Persistent Postural-Perceptual Dizziness (PPPD) may exhibit a wide range of test results, reflecting the complexity of their presentation.
References
[1] Clendaniel R. A. (2000). Outcome measures for assessment of treatment of the dizzy and balance disorder patient. Otolaryngologic clinics of North America, 33(3), 519–533.
[2] Dickins, J. R., Cyr, D. G., Graham, S. S., Winston, M. E., & Sanford, M. (1992). Clinical significance of type 5 patterns in platform posturography. Otolaryngology–Head and Neck Surgery, 107(1), 1–6.
[3] Lacour, M., Tardivet, L., & Thiry, A. (2022). Posture Deficits and Recovery After Unilateral Vestibular Loss: Early Rehabilitation and Degree of Hypofunction Matter. Frontiers in human neuroscience, 15, 776970.
[4] MacKinnon C. D. (2018). Sensorimotor anatomy of gait, balance, and falls. Handbook of clinical neurology, 159, 3–26.
[5] Melillo, F., Di Sapio, A., Martire, S., Malentacchi, M., Matta, M., & Bertolotto, A. (2017). Computerized posturography is more sensitive than clinical Romberg Test in detecting postural control impairment in minimally impaired Multiple Sclerosis patients. Multiple sclerosis and related disorders, 14, 51–55.
[6] Rossi-Izquierdo, M., Soto-Varela, A., Ernst, A., Rubio-Rodríguez, J. P., Santos-Pérez, S., Sesar, Á., Alberte-Woodward, M., Guijarro-Del, M., Román-Rodríguez, E. S., Faraldo-García, A., Zubizarreta-Gutiérrez, A., & Basta, D. (2016). What could posturography tell us about balance problems in Parkinson's disease? Otology & Neurotology, 37(e326–e331).
[7] Shim, D. B., Song, M. H., & Park, H. J. (2018). Typical sensory organization test findings and clinical implications in acute vestibular neuritis. Auris Nasus Larynx, 45(5), 916–921.
[8] Vanicek, N., King, S. A., Gohil, R., Chetter, I. C., & Coughlin, P. A. (2013). Computerized dynamic posturography for postural control assessment in patients with intermittent claudication. Journal of visualized experiments : JoVE, (82), e51077.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
