Subscribe to the Interacoustics Academy newsletter for updates and priority access to online events
Training in Caloric test
Caloric Test: A Deep Dive
Description
This guide provides clinicians with a complete introduction to performing and interpreting the caloric test.
Table of contents
- What is the caloric test?
- Physiology of the caloric test
- Caloric irrigators
- Caloric test procedure
- Caloric test technique
- Caloric test parameters
- Interpretation of the caloric test
- Advantages and limitations of caloric testing
- Practical considerations
- Pitfalls and artifacts
What is the caloric test?
The bi-thermal caloric test was introduced into clinical practice in the early 1940s, mainly because of the development work of Fitzgerald and Hallpike (1942) [1]. It involves introducing a stimulus into an ear which either heats it up or cools it down, creating a temperature gradient. This generates an asymmetry between the two vestibular systems in the inner ears and causes a nystagmus to occur. We call this caloric-induced nystagmus.
When first used, the evaluation of the caloric-induced nystagmus was based upon the observer watching the eye movement and timing the duration of the response. With technological development, later recording techniques such as electronystagmography (ENG) allowed the responses to be quantified in terms of the slow phase velocity and duration of nystagmus eye movements.
In clinics today, the preferred method of eye measurement is videonystagmography (VNG), which has advantages over other techniques, especially as it also allows clinicians the ability to observe the eyes during testing.
Physiology of the caloric test
For caloric testing, you should place your patient in a supine position with their head – or upper body – elevated 30 degrees (Figure 1).
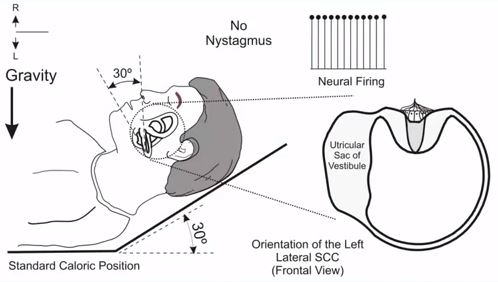
This head position will place the lateral semicircular canals in the plane of gravity. If you look at the patient from the front, you can see the orientation of the semicircular canal. In this case, the left lateral semicircular canal. When there's no irrigation, the neural firing from both the right and left ears are approximately the same. There's no sensation of motion or any type of nystagmus in a normal individual.
The most common method for performing the caloric test is the bi-thermal caloric test. In this method, you irrigate the external auditory canal in each ear twice. Once with a medium (air or water) which is of a slightly higher temperature than the normal body temperature and once with a medium that's slightly cooler than the normal body temperature.
Caloric irrigators
Before we discuss the caloric test in more detail, let’s consider the instrumentation to deliver the caloric irrigations. There are two different kinds of caloric irrigators: open-loop water irrigators and air irrigators. We’ll cover each below.
Open-loop water
This irrigator is called open loop because water goes into the ear canal, and you're supposed to catch it with the basin when it comes back (an open loop). It’s quite easy for the examiner to perform as water will fill the entire ear canal and will cause a robust temperature increase or decrease in the ear. This usually will produce a robust response due to strong the stimulation. It should however be noted that this can be unpleasant for the patient.
The water irrigator by Interacoustics is the Aqua Stim (Figure 2) and has the following temperature range: 30 to 44 degrees Celsius.

Air
The second method of irrigating the ear is to use an air irrigator. Air irrigations have been around for a long time and they're not as messy as open-loop water as there's no water to catch. They're more comfortable to the patient as they don't generate as strong a response. But the downside with air is that it requires more technical skill to administer when compared to water.
There are other things we need to consider with air irrigators. The design of the irrigator tip may affect the temperatures in the ear. So, follow the manufacturer's recommendations. For example, an irrigator where the air freely goes in and out will have a different temperature in the ear canal compared to an irrigator where it seals the ear canal.
Be aware that some air irrigators do not cool the air. They only use the ambient temperature, so if you're in a warm climate, you might not be getting cool irrigations.
The air irrigator by Interacoustics is the Air Fx (Figure 3) and has the following temperature range: 20 to 50 degrees Celsius.

Which kind of irrigator is best?
Use the one you're comfortable with. If you're doing it correctly, both irrigation methods will generate acceptable results with good test, re-test reliability.
Caloric test procedure
Now we’ll cover the test procedure, step-by-step.
1. Assess the ear canal and middle ear
Before completing the caloric test, it’s important to perform otoscopy and tympanometry to assess the status of the ear canal and middle ear. The caloric test compares the results from the right ear to the left ear, so we want the anatomy to be similar on each side.
2. Describe the procedure to your patient
Before putting your patient in the caloric test position, you should first describe the procedure in non‑distressing language. Reassure your patient by explaining that any dizziness experienced is a normal reaction and that the test will not provoke an episode of their own dizziness.
Most patients are worried that they’ll be sick, so you need to reassure them that – in most cases – this will not happen. We’ll address the topic of sickness during caloric testing later in this article as there are procedures that you can follow to reduce patient discomfort.
3. Record spontaneous nystagmus
Once the patient consents to the procedure, it’s important to record any nystagmus in the caloric test position. This is important because if there is a nystagmus present, you should take this into consideration during the results interpretation.
4. Irrigation
You perform the first irrigation with the VNG goggle on the patient with the cover on (vision denied). When the test starts, the irrigator delivers a stimulus into the ear and the software will begin recording the eyes. Depending on the type of irrigation, it either ends after 30 seconds (water irrigation) or one minute (air irrigation). As soon as the irrigation ends, you should engage the patient with some alerting tasks so they're awake and alert throughout the rest of the test.
After 15-30 seconds of irrigation, you will begin to see a nystagmus begin to generate and then increase in size. The response will reach its peak and then starts to subside, which usually occurs about 40 to 45 seconds after the end of the caloric irrigation. Once the response begins to subside, you should ask the patient to fixate.
Most VNG goggles have a light built into them on which the patient can fixate, and you can look at the patient's pupil. When it shrinks, you know that the patient is actually fixating. You do this for about 10-15 seconds and then turn off the fixation light. It’s important to record for a few seconds after the fixation light has been switched off again.
Once the irrigation has finished, you should wait for 5 minutes before starting the next irrigation to ensure the nystagmus has completely stopped.
The test is complete when each ear has received both a warm and a cool irrigation – so 4 irrigations in total.
Caloric test technique
Now, we’ll take a deep dive into the techniques behind warm and cool irrigations.
Warm irrigations
If you start irrigating the external auditory canal with a warm medium (Figure 4), the area of the semicircular canal that's closest to the external auditory canal is going to heat up. In turn, the endolymph in the semicircular canal will get lighter and it will rise. This will put pressure on the cupula and bend it toward the utricular sac.
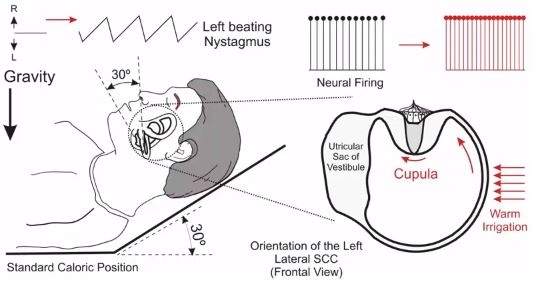
This kind of cupular deflection in the lateral canal would cause excitation of the semicircular canal. In this case, the irrigated ear has a higher neural firing than the non-irrigated ear. That will give the patient a sensation of rotation toward the irrigated ear and the vestibulo-ocular reflex (VOR) will move the eyes away slowly from the irrigated ear.
Then the fast phases of nystagmus will bring the eyes back toward the irrigated ear. In this case, if this is the left lateral semicircular canal, the patient will have left‑beating nystagmus.
Cool irrigations
If you irrigate the ear with a cool temperature (Figure 5), the endolymph will get heavier, and it will sink.

This type of cupular deflection away from the utricular sac will cause inhibition of the semicircular canal and the neural firing will decrease. Because the tonic neural activity in the opposite ear is higher than this, the patient will feel like they're rotating toward the non-irrigated ear or away from the irrigated ear.
Again, the VOR will move the eyes. This time toward the irrigated ear with the fast phases directed away from the irrigated ear.
Cool irrigations will generate nystagmus that beats opposite to the direction of the irrigated ear. Warm irrigations will cause nystagmus to beat toward the irrigated ear. In this example, cool irrigation will cause right‑beating nystagmus as we're irrigating the left ear [2].
Caloric test parameters
There are three important caloric test parameters that we’ll cover in this section:
- Unilateral weakness
- Directional preponderance
- Fixation index
What is unilateral weakness?
Unilateral weakness, also known as canal paresis or reduced vestibular response, is the relative difference between responses from the right and left ears. The terminology that we use is x percentage of unilateral weakness in the weaker ear. For example, we say 64% unilateral weakness in the right ear.
One might consider this value as the gold standard for detecting vestibular abnormalities. The computer calculates this value. You take the total responses from the right ear and subtract the total responses from the left ear. Then, normalize this by dividing it by the total response from both ears.
Here, the total response is 66 degrees per second and the unilateral weakness is 64% (Figure 6).

What is directional preponderance?
Directional preponderance is the relative difference between right‑beating vs left‑beating nystagmus. You take the total right‑beating nystagmus and subtract the total‑left beating nystagmus. Then you normalize it by dividing by the total beating nystagmus from both ears.
Directional preponderance can be caused by two factors. The most common factor is spontaneous nystagmus. The baseline of all the caloric irrigations will shift in one direction based on the slow phases of spontaneous nystagmus. This is the most common method and instead of using directional preponderance to diagnose that, you can make a much easier interpretation based on the spontaneous nystagmus.
There's an extremely rare type of directional preponderance where the irrigation results for one direction of nystagmus are higher compared to the other direction without any substantial nystagmus. Again, an extremely rare finding and we don't know what it means because the incidence of it has been so low that we don't have enough information to judge on that.
What is the fixation index?
The fixation index is a measure of nystagmus intensity during fixation compared to the nystagmus right before fixation. So, we need to do this for both right‑beating and left‑beating nystagmus because fixation suppression can be normal in one direction but not the other. The most common formula is the slow phase velocity right after fixation divided by the slow phase velocity right before fixation.
Analysis and interpretation of the caloric test
In this section, we’re going to go through what a normal caloric response looks like, and common abnormalities seen in the assessment.
Normal results
Figure 7 demonstrates a normal response.

All four caloric irrigations are approximately the same. If you put them in a caloric pod, they all rise from the baseline of zero degrees per second. As the nystagmus slow phase velocity (SPV) is plotted against the time in seconds, you will see the velocity profile of the caloric response has a characteristic shape, rising in velocity before reaching a peak, and then reducing in velocity as the temperature increase caused by the caloric stimulus starts to return to the patient’s normal body temperature.
In a normal caloric response, we would expect the:
- Velocity profile of the caloric response to start to increase in amplitude approximately 20 seconds after the onset of the caloric irrigation.
- Peak nystagmus amplitude at approximately 60 to 90 seconds and then begin to decline.
In the example shown in Figure 7, they all peak around the SPV of 20 degrees per second, after a period of 80 seconds or more, and then decline. It’s reported in the literature that the velocity of the slow phase component of the nystagmus taken at the peak of the caloric response is the useful variable to quantify the caloric reaction [3].
When interpreting the caloric response, you can perform a series of analyses that can answer the questions about the status of the peripheral vestibular system, the lateral semicircular canal function, and the associated central connections. These are:
- Unilateral weakness
- Directional preponderance
- Bilateral weakness
- Hyperresponsiveness
- Fixation suppression
We will now look at these components in more detail.
Unilateral weakness
The most common abnormality in the caloric test is a unilateral caloric weakness (Figure 8).

You can see that the responses from the right ear are much lower than the responses from the left ear. The total response from each ear, signified by the opening of this pod, is much smaller for the right ear. That indicates a unilateral weakness in the right ear. In the calculations, you can see a 64% unilateral weakness in the right ear, above the criterion for abnormality of 25% (some use 20%).
All the tests are centered around zero, which means this patient has no spontaneous nystagmus. Thus, this is likely a chronic lesion or a statically‑compensated lesion. If it was an acute lesion, you'd see all the irrigations shifted to one direction due to the presence of a spontaneous nystagmus.
What can cause a unilateral weakness?
Unilateral weakness is a peripheral vestibular lesion involving the lateral semicircular canal or its efferent pathways on the weaker side, which is usually the superior part of the vestibular nerve. This can be caused by diseases that affect the labyrinth, the vestibular nerve, or the blood supply to those sites.
In an uncompensated or acute version of this, it could be:
- Vestibular neuritis
- Viral or bacterial labyrinthitis
- Initial episodes of Meniere's disease
- Labyrinthine concussion or infarction
In a compensated or chronic version of this, it could be:
- Vestibular neuritis
- Viral or bacterial labyrinthitis
- Late stages of Meniere’s disease
- Vestibular schwannoma or acoustic neuroma
Central lesions that affect the root entry zone of the vestibular nerve – such as multiple sclerosis (MS) – can cause unilateral weakness but other central‑nervous‑system (CNS) signs will also be present.
Directional preponderance
For directional preponderance, most people use 30% as the limit between normal and abnormal. It doesn't have any value for localization. You may be better off looking at the spontaneous nystagmus rather than directional preponderance.
In Figure 9, the patient has 9 degrees per second of left‑beating, spontaneous nystagmus. That's a significant amount of spontaneous nystagmus and you should consider it as abnormal. When measured in the caloric position, you can use the spontaneous nystagmus velocity and direction to correct the measured caloric responses to verify whether a true unilateral weakness is present. In Figure 9, you can see the effect of the 9 degrees per second of left‑beating, spontaneous nystagmus the most in the left cool caloric irrigation, which is corrected in the calculation for caloric asymmetry.

Bilateral weakness
The next abnormality is bilateral vestibular weakness, also known as hypofunction or hyporesponsiveness. There are different criteria, but in this case, we’ll use a total response in each ear of less than 12 degrees per second. If you look at this patient, they are abnormal (Figure 10).

What does bilateral caloric weakness mean?
In reality, not much. You have to do a secondary test to confirm a bilateral vestibular loss. This is due to the heat transfer issues mentioned earlier. For example, if somebody has bilateral otosclerosis, the heat doesn't reach the labyrinth. If the heat transfer is disrupted through the middle ear, this can result in what appears to be a bilateral weakness, but this doesn't mean that the vestibular system is abnormal, as the caloric stimulus might not have reached the end organ.
In cases of suspected bilateral vestibular weakness, you always must do a secondary test. The gold standard would be a rotational chair – at least in the past. These days, video head impulse testing (vHIT) is much less costly and occupies a much smaller area, so you might try a vHIT goggle.
In the old days, we used to do bilateral ice water testing. We don't do that anymore and it's not recommended. If either the rotational chair or video head impulse test confirm the bilateral weakness as a bilateral vestibular loss, then you can conclude that the patient has a hyporesponsiveness / hypofunction in the semicircular canals of both peripheral vestibular systems.
You can perform another cross‑check by assessing otolith function with vestibular evoked myogenic potentials (VEMP). Utilizing cervical and ocular VEMP in the assessment of peripheral vestibular function allows us to determine if the gravity‑sensing organs of the peripheral vestibular system are also indicating reduced or absent function.
What can cause bilateral weakness?
Often, it's a bilateral loss of peripheral function in both ears, but you can also have central abnormalities that cause bilateral weakness. For example, if somebody has a tumor at the cerebellum, that's blocking the neural firing from reaching the central nervous system. These patients might have a bilateral vestibular loss.
The most common etiology is unknown, but among the known causes are:
- Idiopathic
- Ototoxicity
- Bilateral Meniere's disease
- Cerebellar degeneration and tumors
- Congenital malformations such as Chiari malformation
Hyperresponsiveness
Hyperresponsiveness, also known as hyperactivity or hyperfunction, is a rare finding in the caloric test. The criterion is not very clear. We can use the hyperactive response criteria published by McCaslin in 2019 [4].
- Total cool peak response (left cool plus right cool) is more than 99 degrees per second
- Total warm peak response (left warm plus right warm) is more than 146 degrees per second
- Total peak response (total cool plus total warm) is more than 221 degrees per second
In Figure 11, the total responses from both ears are high at 263 degrees per second, with the total warm being 152 degrees per second, and the total cool being 111 degrees per second. This suggests the caloric response recorded in Figure 11 is exhibiting hyperactive characteristics.

If you determine that the hyperactivity is real, and you have ruled out any historical middle ear or mastoid surgery that might expose the labyrinth, then it denotes a central lesion. It's most likely due to the loss of inhibitory responses at the vestibular nuclei. It's seen in patients with cerebral atrophy and diseases that affect the cerebellum. It's also been reported to a lesser extent in patients with migraine and motion sensitivity syndrome. This is understandable as there is some cerebellum involvement in these patients, so you would expect them to have strong responses to caloric irrigations.
Failure of fixation suppression
The next abnormality is the failure of fixation suppression. The criterion is a fixation index of either 60% or 50%. If it exceeds that, you should consider it abnormal. In this patient, especially for right irrigations, the fixation suppression is abnormal (Figure 12).

For both directions of nystagmus, this patient would also likely have some form of tracking abnormality in the smooth pursuit test.
One thing you must make sure is that the patient is actually looking at the target. One quick way of determining that is observing the patient's pupils when the light turns on. If the patient's pupils shrink, that means the light is being observed, but the patient still must concentrate to suppress the nystagmus generated in the caloric test. Once you determine that the patient is concentrating and looking at the target, this type of abnormality is failure of fixation suppression.
It has the same significance as smooth pursuit abnormalities. It's a central lesion that could be in different parts of the central nervous system:
- Pons
- Cerebellum
- Parietal-occipital cortex
It's most common in patients with midline cerebellar abnormalities.
Advantages and limitations of caloric testing
As we have covered caloric testing equipment and the caloric test procedure, let’s cover the advantages and limitations of caloric testing.
Advantages
Unlike head movements, you can deliver caloric irrigations to each labyrinth independently. That makes it very effective for detecting unilateral vestibular losses. Also, you can generate caloric stimulation with relatively small and inexpensive equipment, compared to a rotational chair for example.
Limitations
Caloric testing also has some limitations that you should be aware of.
1. The responses are not calibrated
This means the responses vary from one person to another. Sometimes, even from one ear to the other. This is because – as we have discussed – the whole basis of the caloric test is the heat transfer from the external auditory canal, through the middle ear to the labyrinth. This heat transfer therefore depends on the anatomy and other factors.
This means if one person has a peak response of 20 degrees per second and another person has a peak response of 10 degrees per second, you can't say that one person's labyrinth is more sensitive than the other because it might be that the heat transfer is not as effective in one person compared to the other.
2. It’s a test of the lateral semicircular canals
Technically, you can put the anterior and posterior canals in the plane of gravity and try to do caloric testing. But they're far too embedded in the temporal bone, so the heat transfer is diminished. The caloric test is primarily considered as a test of the lateral semicircular canals and the superior part of the vestibular nerve.
3. Very low-frequency stimulation
Caloric testing generates very low‑frequency stimulation, which is not in the physiological range of the vestibular system. For example, the rotational chair in the sinusoidal harmonic acceleration test can go from a very low frequency such as 0.1 up to 1.28 Hz, which is in the physiological range of the human VOR. The caloric test is referred to in the literature as an extremely low‑frequency test, at a frequency equivalent to 0.004 Hz [5].
4. Not well tolerated
Another limitation is that the patients usually find the caloric test distressing. As it’s one of the few vestibular tests that induces a conflict between the output (efferent) signals from the peripheral vestibular system, it will make the patient experience a sensation of movement, often described as dizziness, and is not well tolerated by some.
5. Bilateral vestibular hypofunction
Finally, what makes it attractive for unilateral vestibular hypofunction, where we compare the right and left ears, is a limitation when it comes to abnormalities that affect both vestibular systems. For example, caloric testing is not the most effective test in patients with bilateral vestibular hypofunction.
Practical considerations
Now, let’s cover some practical considerations when performing caloric irrigations.
Calibration between irrigations
In the old days and to this day, the ANSI recommendation is that you calibrate eye movements between irrigations. The British Society of Audiology, which also has standards for caloric testing, matched the ANSI standards early on but have later reversed their recommendation when the eye movement measurement technology moved to VNG.
The ANSI recommendation is for ENG and non‑computerized, strip‑chart recording systems. For VNG, calibration between irrigations might actually create more variability, so it's not recommended. If you have a good calibration, it’s generally unnecessary to carry out further calibration, unless you move the cameras within the goggles or if you remove or reposition the goggles.
Order of irrigations
Both ANSI and BSA recommend that you start with the warm temperature. That's a good recommendation, especially if you decide to do just two irrigations. In other words, if you want to do monothermal calorics, they are more effective with warm irrigations.
There's a good basis on why you should start with warm. A study by Noaksson et al. in 1998 [6] showed that if you start with warm, which is an excitatory response, the very first irrigation is usually stronger than the rest. This causes a bit of a temperature effect. Usually, warm irrigations are stronger than cool irrigations.
The 1998 study shows that if you start with cool irrigations, the difference is reduced. So, if you're going to do all four irrigations, it might be best to start with cool. But if you ever think that you're going to stop after two irrigations, then definitely start with warm.
Wait period between irrigations
As for how long you should wait between irrigations, ANSI recommends a fixed period of time of around five minutes between the start of consecutive irrigations. This recommendation doesn't differentiate between a person who has a very strong response and somebody who has a weak response.
The British Society of Audiology recommends a minimum interval of seven minutes between the start of consecutive irrigations. Seven minutes and longer is usually enough, even in a patient who has a strong response.
To save some time, you can wait for the previous caloric nystagmus to subside. From that point on, wait a fixed amount of time of 3-5 minutes. You can then check for any residual nystagmus by assessing eye movements with fixation removed. This will ensure that the effect of the previous irrigation has subsided before starting the next irrigation.
Should you use air irrigators?
If you’re using an air irrigator, you might be interested to know that in the USA, ANSI disapproves the use of air as a mode of irrigation. They recommend either open-loop or closed-loop water. However, closed-loop water systems are no longer manufactured.
Clinicians have not followed the recommendation, with a ratio of air to water irrigator sales at about four to one. It seems clinicians prefer air, and this is likely due to its advantages as we discussed before.
How many tests for fixation suppression?
At least two, one for each direction of nystagmus. But it's best if you do this for all four irrigations. By doing so, you can choose the two irrigations where the nystagmus intensities right before the irrigation are approximately the same. That's a fair comparison and how you should compare fixation suppression for the right and left.
Are monothermal irrigations enough?
If you use the standard parameters, your false positive rate will be very high. You’ll also miss the opportunity to identify some of the artifacts. It’s possible to use monothermal warm calorics as a screening test, primarily to identify normal calorics.
A study by Murnane et al. in 2009 [7] has laid out the parameters that must be satisfied for this type of test:
- No oculomotor abnormalities
- No gaze-evoked or spontaneous nystagmus
- The difference between peak responses should be less than 10%
If all these three conditions are met, then it's very likely that your calorics are normal and you can stop after two irrigations. You can relax these conditions a bit if you're including another test. For example, if you have a vHIT which is normal, then two irrigations are probably adequate if they also show a minimal amount of asymmetry.
How do you reduce the risk of the patient feeling sick?
Usually, most of the discomfort occurs during the first irrigation. If the patient can manage the first irrigation, they are likely going to be okay for the rest of the irrigations. Pay attention to your patient's body responses. If their breathing intensifies and you can feel the heat rising from the patient's body, then you know that the patient is under a bit of distress.
If you get to a point where you feel like the patient might get sick, interrupt the irrigation and make a note of the time. For example, if you were in the middle of a one‑minute irrigation, but you only did 40 seconds, make a note of 40 seconds and allow time for the patient to recover. After that, perform 40-second irrigations for all the remaining irrigations.
If the patient is getting too distressed, you can sit the patient up and turn the head 30 degrees downward. That will place the lateral canals in the horizontal plane. This will stop the endolymph flow and the patient might recover quicker. Of course, you have to do that before the patient gets to a point of no return.
Vertical nystagmus during caloric testing
Vertical nystagmus is quite common, both in normal individuals and patients with different abnormalities. The most likely cause of this is that a slight amount of stimulation reaches the posterior and anterior canals, from which vertical nystagmus originates.
In the old days, there was some discussion over caloric perversion. In caloric perversion, by definition, all four irrigations must generate either purely vertical nystagmus or vertical nystagmus that's much stronger than the horizontal nystagmus. Caloric perversion is a central abnormality, but it's extremely rare. In most cases, there's a much simpler explanation than caloric perversion.
Is there an age limit for caloric testing?
There's no upper age limit, but you should realize that irrigations may not be as effective in older patients. Due to the thickening of the tympanic membrane, otosclerosis or other middle ear changes, caloric irrigations might generate minimal responses.
You might think that the patient has a bilateral weakness, a deterioration of the vestibular system due to age. But in most cases, if you test the patient with a different mode of vestibular stimulation like rotation or vHIT, you'll see that these patients have normal responses. So, it's most likely because of heat transfer issues in older individuals and you should be aware of that.
The lower age limit is five years of developmental age in children and adults with developmental delays. If the patient is cooperative, you can go a bit lower than that. If the patient isn't cooperative, you probably have to go higher than that. If somebody calls and asks if you can test a two-year-old child, the answer is most likely no. Children that age do not let you put an irrigator in their ear and hold it there for such a long time. So, caloric testing is not an optimal test in the pediatric population.
Learn more: Pediatric vestibular assessment (rotational chair focus)
Pitfalls and artifacts
By its nature, caloric testing is susceptible to artifacts. We must make sure that we eliminate or recognize them before we interpret them.
1. Verify nystagmus beats
One of the things that happens in the computer analysis is that it tries to verify or identify nystagmus beats and then determine the slow phase velocity of those nystagmus beats. That process is never perfect regardless of which system you use. There are occasionally nystagmus beats that are either missed or falsely verified.
You must make sure that the nystagmus beats are cleaned up and they actually represent the slow phase velocities. When you do that, remember that consecutive nystagmus beats can't be more than a few degrees apart. If one nystagmus speed shows 20 degrees per second, and the one next to it shows 5 degrees per second, then one of them is not right.
Usually, the one that has more neighbors is the one you should consider. During this process, make sure you remove clear outliers to clean up your tracings and get a better representation of the average slow phase velocity of the measured nystagmus.
2. One irrigation is a lot different than the other three
Another type of artifact is when one irrigation produces results that are very different than the others. It would be prudent not to interpret it. If you do, it will show something that's abnormal. If you repeat the outlier irrigation, it will usually produce results similar to the other irrigations.
On occasion, one irrigation is much larger than the rest. That is typically the first warm irrigation. Again, try repeating the outlier irrigation. If it doesn’t change, repeat the other temperature on the same side, as there may have been inadequate irrigation. One way or the other, by repeating, the weakness will increase, indicating a true unilateral weakness, or it will decrease, indicating a normal finding.
Summary
Even though the caloric test doesn't identify a specific etiology, it's proven to be the most useful test for detecting unilateral vestibular lesions. With the introduction of the vHIT, the need for doing a full, bi‑thermal caloric test has somewhat diminished. But in some cases, the caloric test is still the only test that can determine the side of lesion with a high level of confidence.
The research literature suggests that in some peripheral pathologies, such as endolymphatic hydrops, the caloric test may show changes in the sensitivity of the peripheral vestibular system in the early stages, so it remains a valuable tool in vestibular diagnostics.
Related courses
References
[1] Fitzgerald, G., Hallpike, C. S. (1942). Studies in human vestibular function: I. Observations on the directional preponderance ("Nystagmusbereitschaft") of caloric nystagmus resulting from cerebral lesions. Brain, 65(2), 115–137.
[2] Barber, H. O., & Stockwell, C. W. (1980). Manual of Electronystagmography. St. Louis, MI: CV Mosby.
[3] Jacobson, G., Newman, C., Peterson, E., Jacobson, G., Newman, C., & Kartush, J. (1993). Handbook of Balance Function Testing.
[4] McCaslin, D. L. (2019). Electronystagmography and Videonystagmography (ENG/VNG). Plural Publishing.
[5] Shepard, N. T., Jacobson, G. P., Furman, J. M. (Ed.), & Lempert, T. (Ed.) (2016). Chapter 9 - The caloric irrigation test. In Handbook of Clinical Neurology (Vol. 137, pp. 119-131). Elsevier.
[6] Noaksson, L., Schulin, M., Kovacsovics, B., & Ledin, T. (1998). Temperature Order Effects in the Caloric Reaction. The international tinnitus journal, 4(1), 71–73.
[7] Murnane, O. D., Akin, F. W., Lynn, S. G., & Cyr, D. G. (2009). Monothermal caloric screening test performance: a relative operating characteristic curve analysis. Ear and hearing, 30(3), 313–319.
Presenter

Get priority access to training
Sign up to the Interacoustics Academy newsletter to be the first to hear about our latest updates and get priority access to our online events.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
