Join the Interacoustics community and receive news about new products, events and much more
Vestibular function testing during head movement
Functional assessments can be a useful measurement of vestibular performance during head movement.
They can reveal why the patient might have troubles reading or focusing on targets during head movement and identify whether dizziness is connected to specific head speeds.
There are many different functional tests, but I will focus on two tests you can perform with VisualEyes™:
- Lateral Head Roll
- Dynamic Visual Acuity
But first, let’s look at a very common manifestation of dizziness.
Author's note: Throughout this article, I'll be referencing a video recording of a presentation I held in October 2020, with time stamps for the example in question. I recommend watching the portions of the video that I reference to for best learning outcomes.
Benign Paroxysmal Positional Vertigo (BPPV)
BPPV is a very common abnormality and has several variants.
One such variant is horizontal canal BPPV, which causes dizziness with back- and forth head movements.
This would make driving a car very difficult, right?
This variant of BPPV is often a result of an improper maneuver to correct the simpler posterior canal BPPV.
So, it is important to have the correct tools to assure correct patient head position, and accurate eye tracking algorithms to assure correct diagnosis.
Cammy Bahner, AuD, has addressed posterior canal BPPV diagnosis, so I will show you a case of horizontal BPPV instead, using the Lateral Head Roll test.
Lateral Head Roll case
In this portion of the video, the patient is supine and rolls her head to the right.
The maneuver guide has a bar that indicates correct patient head position by turning green.
If the patient’s head is turned to the right, we see right-beating horizontal nystagmus, and vice versa.
In this case it is geotropic nystagmus, which lets the examiner know that crystals are present in the horizontal canal.
When the test stops a bar graph pops up, which gives us a quick glance to know which side is affected.
In this case 6 degrees of right-beating nystagmus and 11 degrees of left-beating nystagmus.
Given their relative values and the fact that 6 degrees is the cutoff for normal, we can conclude that this patient has stronger nystagmus when her head is rolled to the left.
Thus, the left lateral canal is the affected canal.
Key takeaway: The Lateral Head Roll test is a simple but accurate tool.
Multivariant BPPV
To take the Lateral Head Roll case one step further, observe this portion of the video.
If we look at the graph that says vertical left, we can see a few small beats of up-beating nystagmus.
Alongside 6-degree horizontal nystagmus, the data does not qualify as abnormal.
Although, the data still triggers an alarm bell.
The patient may have multi-canal involvement, maybe posterior and lateral canal involvement (multivariant BPPV).
This can be tricky to treat with manual treatment methods.
But, by utilizing the TRV Chair, we can treat multivariant BPPV.
The chair allows the examiner to precisely maneuver the patient while providing little shocks.
The resulting kinetic energy can move the crystals back to the utricle efficiently.
Key takeaway: The TRV Chair’s kinetic energy offers an alternative to manual treatment and provides more accurate repositioning.
Vestibulo-ocular reflex (VOR)
Why has the world gone blurry?
Imagine if you could not read words clearly when you turned your head.
That could be a problem in so many different situations.
Why does this happen?
Well, the vestibulo-ocular reflex (VOR) is what keeps our eyes on the target during head movement.
Thus, the VOR serves to maintain visual acuity during head movements.
When we walk, run, or turn our heads, we want to maintain a clear view of the world.
This is necessary for both orientation and self-preservation.
If the VOR is damaged, then the world goes blurry when we move our heads.
This is where the Dynamic Visual Acuity (DVA) test comes into the picture.
Snellen eye chart
Before computerized DVA systems were available, clinicians used Snellen eye charts mounted on the wall.
This method compares the lowest (smallest) line a person can read, making less than 3 errors, while the head is static versus rapid head movement.
The benefit of the Snellen eye chart is that you can easily perform this test in children as well as adults.
There are some drawbacks though:
- Hard to control head speed
- Cannot separate directional acuity
- Not objective
- No numerical values
The above drawbacks prevent us from monitoring functional improvements over time.
Let’s move on to computerized DVA.
Computerized DVA
So, a better, more objective way to measure dynamic acuity is to use computerized DVA systems.
I have provided an example in this portion of the video.
In computerized DVA, the patient wears a headband attached with a sensor.
The software plays a metronome sound, and the patient is instructed to move their head to the beat (either a horizontal or vertical movement).
The test can be performed on a small laptop or a large TV screen, depending on the clinical need and infrastructure.
If the patient moves their head at the correct velocity, an optotype pops up on screen.
The fact that the optotype only pops up at correct head velocity is key to the computerized method’s objectivity.
Using a remote control, the patient must then press which way they think the optotype is pointing.
Key takeaway: Computerized DVA is more accurate than the manual Snellen eye chart.
Computerized DVA test procedure
Please observe this portion of the video.
First, the head is static with no sound (metronome).
The patient is just pressing the button to tell the clinician which way they think the optotype is pointing.
This produces a static acuity score.
For dynamic acuity, the patient is instructed to move their head in beats that align with the metronome.
The guide bar turns green when the velocity is correct, and the patient is again tasked with pressing the remote control to tell which way they think the optotype is pointing.
This produces a dynamic acuity score that can be compared with the static acuity score.
If dynamic acuity is much worse than static acuity, then we know the patient has difficulty keeping vision clear while in motion.
Computerized DVA case study
A patient of mine came in on day 1, complaining of dizziness when moving his head.
I performed the DVA test, summarized in Figure 1.
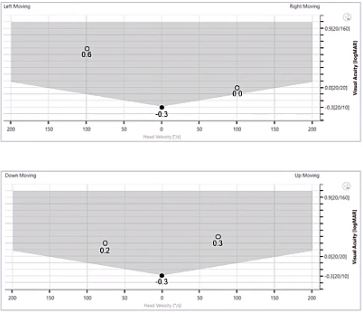
Figure 1: DVA results before rehabilitation. Abnormal scores lie within grey shaded area.
He had poor scores when moving his head to the left, accompanied by better but still abnormal problems to the right and up and down.
I sent him away to do gaze stabilization exercises for a week and a half.
Upon return his scores had improved but he was not fully rehabilitated. Upon second return a week and a half later, he was completely normal (Figure 2).
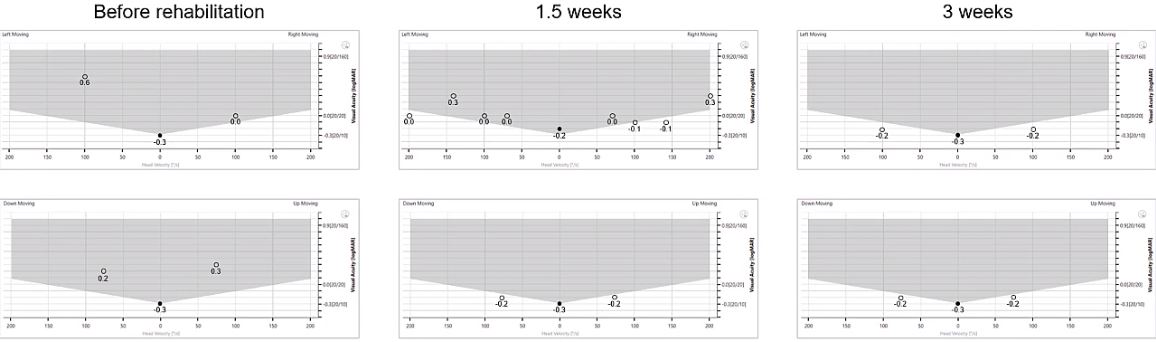
Figure 2: DVA results before, during, and after rehabilitation. Fully rehabilitated after 3 weeks.
Key takeaway: Computerized DVA is a good test to measure vestibular compensation over time.

Similar Topic
Stay up to date!
Subscribe to our newsletter and receive news on new products, seminars and much more.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
