Join the Interacoustics community and receive news about new products, events and much more
2 ways to improve posterior canal BPPV diagnosis
It can often be very difficult to diagnose posterior canal BPPV when relying on two-dimensional graphs that only show horizontal and vertical eye traces.
It can also be difficult for the examiner to know if they have placed the patient’s head in the correct position for an effective Dix-Hallpike evaluation.
In the below, whether you favor to watch or to read, I will show how you can use VisualEyes™ to solve both of these challenges.
1. Use the 3D head model to be sure of correct patient head position
Let’s look at the latter of the two challenges first.
The advanced Dix-Hallpike maneuver uses a head sensor that attaches to the goggles and can detect the patient’s head position in any plane.
The 3D head model built into the VORTEQ™ Assessments module in VisualEyes™ will then represent the patient’s head position as soon as you have calibrated the sensor.
There is a target graph above the head model with an indicator that allows the examiner to see when they have the patient’s head turned to precisely 45 degrees right or left.
The second target graph to right of the head model allows the examiner to see when they have lowered the patient’s head to the correct hanging position (Figure 1).
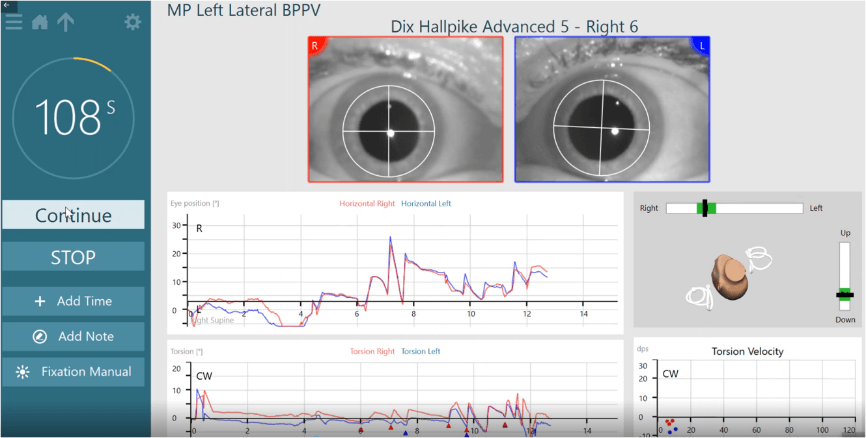
Figure 1: VisualEyes™ maneuver guides.
The indicators turn green when the head is within the acceptable angle.
This precision provided by the 3D model takes the guesswork out of the evaluation, gives the examiner confidence, and ultimately leads to better posterior canal BPPV diagnoses.
2. Use torsional eye tracking
Relying solely on horizontal and vertical eye traces is problematic when the nystagmus elicited by posterior canal BPPV is torsional in nature.
Thus, in cooperation with Johns Hopkins, we have developed a torsional eye tracking algorithm and implemented it in VisualEyes™.
This allows you to visualize the torsional components of the eye movement, as well as measure and extract the torsional direction and velocity throughout the duration of the maneuver.
How to set the reference for successful torsional tracking
Setting the reference on the iris of the eye is paramount to successful torsional tracking.
It is quick and will save time throughout the evaluation if done correctly at the onset.
But how do you do it correctly?
If the reference for torsion is set when the goggle cover is off (Figure 2), the pupils will be too small, as will the reference area.
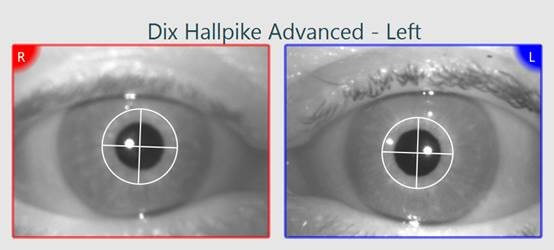
Figure 2: Wrong way of doing torsion calibration. Goggle cover is off.
For best tracking conditions, set the reference in the same condition as you will perform the test; with the patient wearing the light-tight fixation-free goggle cover (Figure 3).
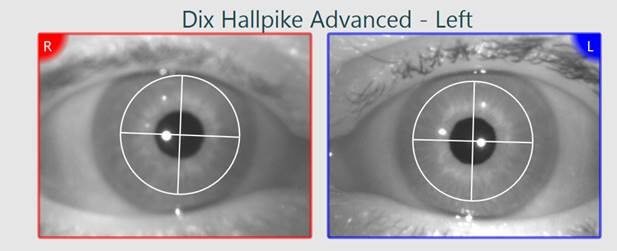
Figure 3: Correct way of doing torsion calibration. Goggle cover is on.
Torsion velocity graph
Since torsional eye movements are the most important part of a Dix-Hallpike maneuver, VisualEyes™ brings this to the forefront.
You will see the data points for each identified beat of torsional nystagmus plotting in the torsion velocity graph in real-time through the exam (Figure 4).
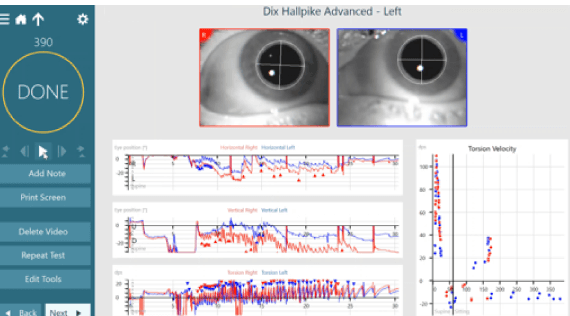
Figure 4: Patient with left posterior canal BPPV confirmed with 3D eye movement analysis including torsional eye movements.
Again, this adds confidence for the examiner, especially in those cases where it is difficult to visually observe the torsional nystagmus in the eye video.
This will often be the case, where the torsional nystagmus is so small that it is difficult or even impossible to rely on the video alone.
The torsional algorithm can measure nystagmus as small as 1 degree, providing clinicians with the precision they need.
The video playback screen allows you to see all the data for the horizontal and vertical eye movements, which is still important.
But by adding the third component of torsion we can fill in the gaps that have been missing with traditional Dix-Hallpike testing.
Torsional data is useful for differential diagnosis
The added torsional tracking not only helps you in your diagnosis of posterior canal BPPV, but the lack of torsion is equally as important for differential diagnosis.
Let’s look at this case example (Figure 5).
If you look at the horizontal and vertical eye traces and SPV graphs, you can see that this patient had 7 deg/sec left-beating nystagmus and 3 deg/sec up-beating nystagmus during the left Dix-Hallpike evaluation.
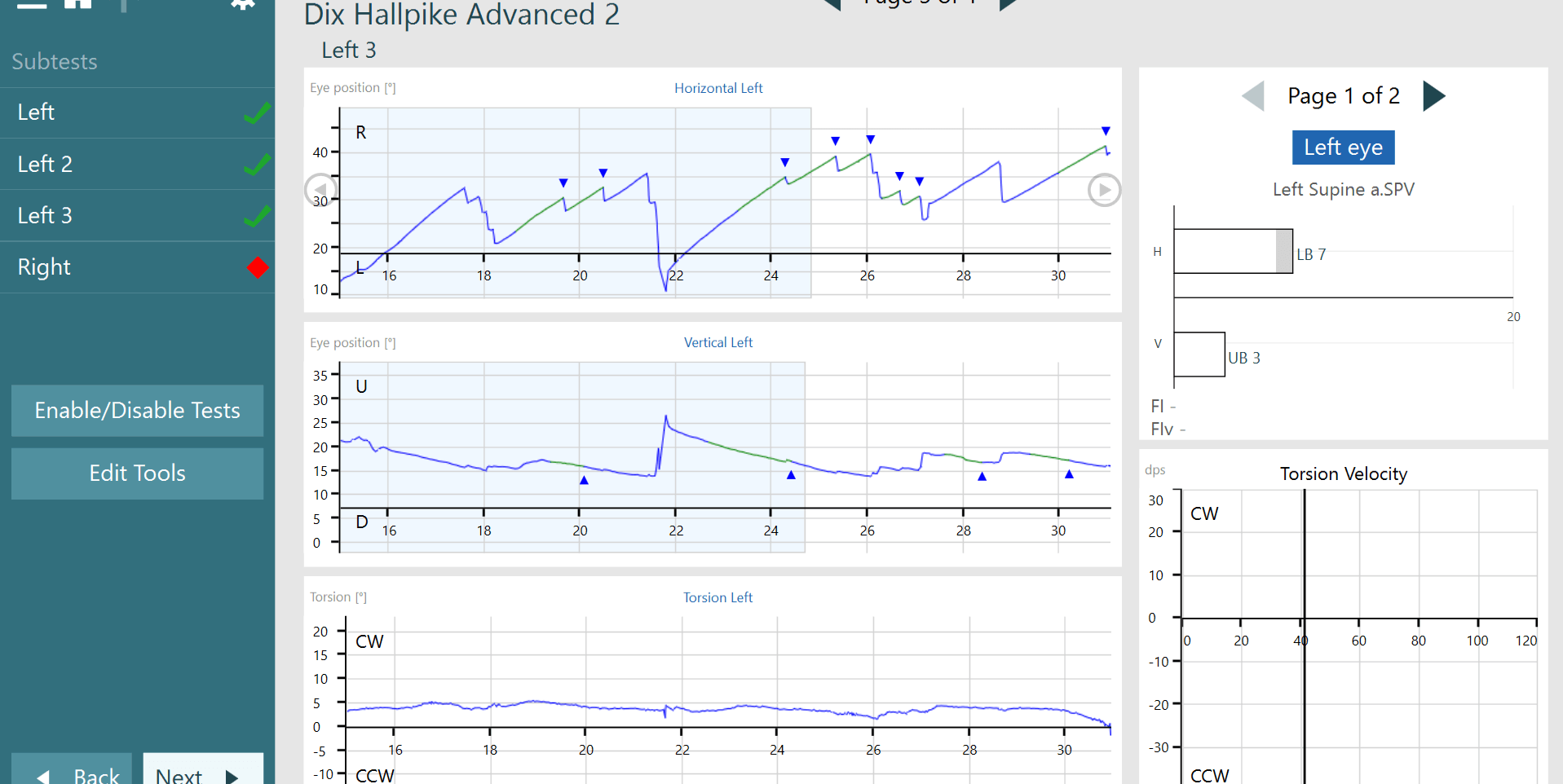
Figure 5: Patient with a central lesion resulting in positional nystagmus. Not BPPV as there is no torsional component present.
Upon inspection of those graphs only, you may believe this patient has a mild left posterior canal BPPV.
Yet, if we look at the torsion trace and torsion velocity graph (Figure 6), you can see that there are no identified beats of torsional nystagmus.
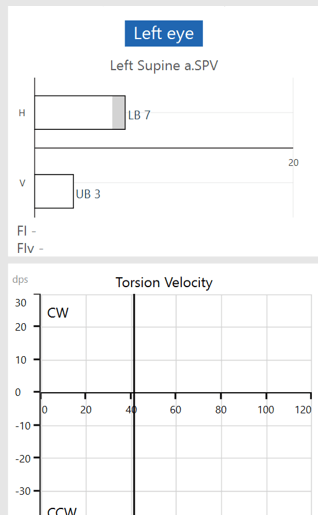
Figure 6: A central vestibular test finding with no torsional nystagmus present.
The lack of torsion in this case helps the examiner to avoid a misdiagnosis.
This patient was diagnosed with central positional vertigo, as evidenced by horizontal and vertical eye traces, along with no visible torsional nystagmus in the additional graphs.
This again highlights the benefit of recording all three components of eye movement.
Conclusion
In summary, you can see how important it is to have these extra tools to assure you are making the most accurate diagnosis as possible.
Without the head model guides we can only approximate the correct position of the patient during the maneuver.
Without the torsional analysis we are often left to try and ‘guess’ if there was actual torsional nystagmus present or not.
Taking the ‘guesswork’ out of the examination allows us to make a more certain assessment.
The better the assessment, the more successful we will be at treating this patient’s condition.
It is our responsibility as clinicians to provide the best diagnosis and treatment outcomes that we can.
Thus, having the proper tools to do this is imperative to the success of our clinics.

Similar Topic
Stay up to date!
Subscribe to our newsletter and receive news on new products, seminars and much more.
By signing up, I accept to receive newsletter e-mails from Interacoustics. I can withdraw my consent at any time by using the ‘unsubscribe’-function included in each e-mail.
Click here and read our privacy notice, if you want to know more about how we treat and protect your personal data.
